1. Introduction
Colorectal cancer (CRC) is a major public health problem, associated with high morbidity and mortality rates in the West. CRC represents the end point of a wide range of genetic and epigenetic changes that occur in normal colorectal cells.
It is estimated that approximately 85% of CRCs develop from colorectal polyps. Adenomatous polyps and sessile serrated lesions (SSLs) are the most important precursors of CRC. It is estimated that adenomas and SSLs are present in 20% to 50% of individuals over 50 years of age [1].
2. WHO Classification for Colorectal Serrated Lesions
Until 2010, colorectal serrated lesions were generally considered harmless lesions and reported as hyperplastic polyps (HPs) by pathologists and gastroenterologists.
Subsequently, a variety of terms were used to describe these lesions, contributing to misunderstandings about the terminology and classification of serrated lesions.
In 2010, the World Health Organization (WHO) proposed the following classification for colorectal serrated lesions (4th edition = penultimate version until the publication of this article):
| Histological Type | Histological Type |
|---|---|
| Hyperplastic Polyp (HP) | • Microvesicular Type |
| • Goblet cell-rich Type | |
| • Mucin-poor Type | |
| Sessile Serrated Adenoma/Polyp (SSA/P) | • SSA/P with dysplasia |
| • SSA/P without dysplasia | |
| Traditional Serrated Adenoma (TSA) |
In 2019 the WHO updated the classification of Colorectal Serrated Lesions (5th Edition) [2]. This new classification differentiates serrated lesions into four categories:
| Histological Type | Subtype Histological |
|---|---|
| Hyperplastic Polyp (HP) | • Microvesicular Type |
| • Goblet cell-rich Type | |
| Sessile Serrated Lesion (SSL) | • SSL |
| • SSL with dysplasia (SSLD) | |
| Traditional Serrated Adenoma (TSA) | |
| Serrated Adenoma, Not Classified |
The main change in terminology is the approval of the new term “sessile serrated lesion ” (SSL), which aims to adjust the previous confusing terminologies “sessile serrated adenoma and sessile serrated polyp “. Indeed, the term “adenoma” includes the concept of dysplasia, which is not observed in a significant number of SSLs. Now, when the pathologist observes a dysplastic pattern in SSLs, they should use the terminology “SSL with dysplasia”. Moreover, a large part of SSLs do not have a polypoid appearance, making the term “polyp” inappropriate.
3. Colorectal Serrated Lesions: Histological and Endoscopic Characteristics
Microscopically, colorectal serrated lesions are characterized by the presence of serrated folds similar to saw teeth in the epithelial crypts [1]. The differences between the main subtypes of serrated lesions lie in the architectural characteristics and the location/extent of the proliferative zone.
3.1 – Hyperplastic Polyps (HP)
- HPs are the most common serrated lesions, representing about 75% of all serrated polyps.
- Estimated prevalence in patients undergoing screening colonoscopies is 20–30%.
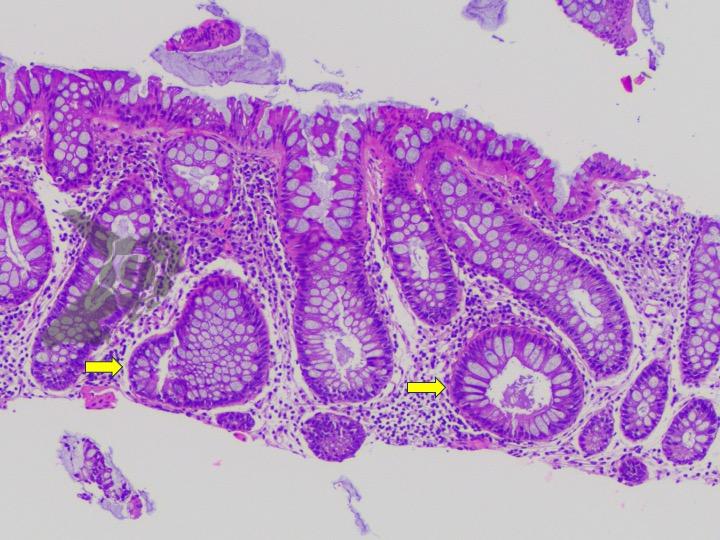
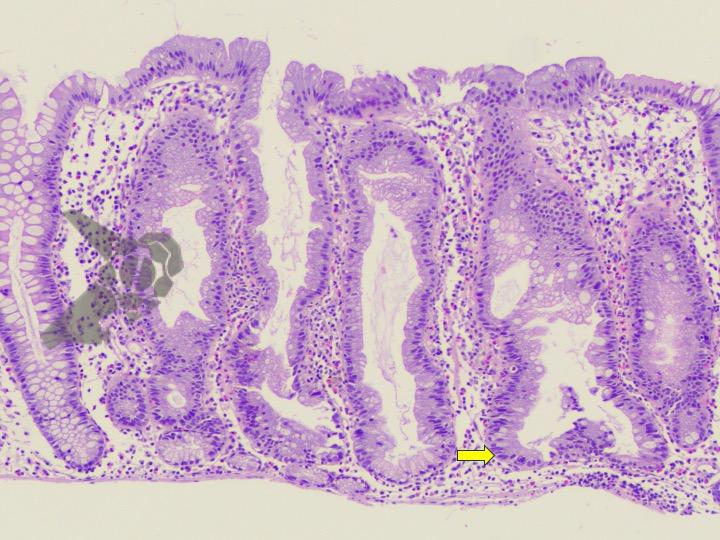
- In HPs, the crypts are straight and elongated, with a serrated architecture confined to the upper two-thirds of the crypts and the cells show minimal cytological atypia.
- At the base of the crypt, the architecture is regular and not serrated, and the cells do not show signs of atypia.
- HPs are commonly found in the left colon, mainly in the rectosigmoid colon, and usually measure less than 5 mm.
- In white light endoscopy, they appear as raised or sessile lesions, sometimes covered with normal mucosa.
- In chromoendoscopy, a type II star-shaped crypt pattern is observed on the surface of the lesion.
There are two variants of Hyperplastic Polyps:
- microvesicular type hyperplastic polyps:
- characterized by the presence of small mucus droplets in the cells
- considered precursors of SSL.
- goblet cell-rich hyperplastic polyps:
3.2 – Sessile Serrated Lesions (SSL)
- SSLs are the second most common type of serrated lesion and are considered precursor lesions of CRC. (More etiopathogenic details)
- The prevalence of SSL in the general population is 5–10%.
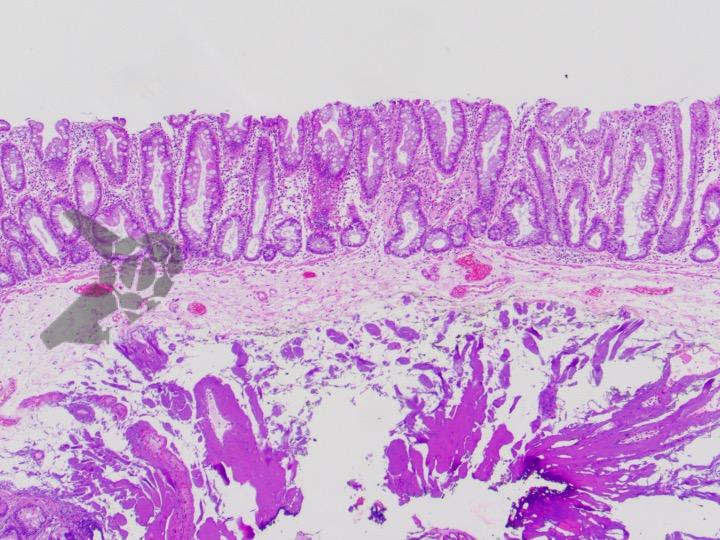
- Generally, SSLs are larger than HPs, with an average diameter between 5-7 mm, and their shape is flat or sessile.
- Unlike HPs, SSLs are more frequent in the right colon.
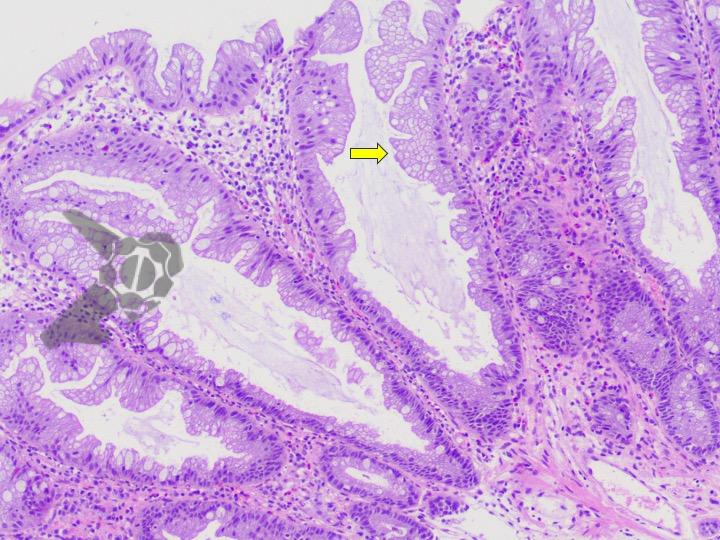
- The histological characteristic that distinguishes SSL from HP is the presence of distorted serrated crypts.
- For the histological diagnosis of SSL, the crypt must show at least one of the following characteristics:
- Horizontal growth along the muscularis mucosae.
- Dilation of the base of the crypt.
- Serration extending to the base of the crypt.
- Asymmetric proliferation.
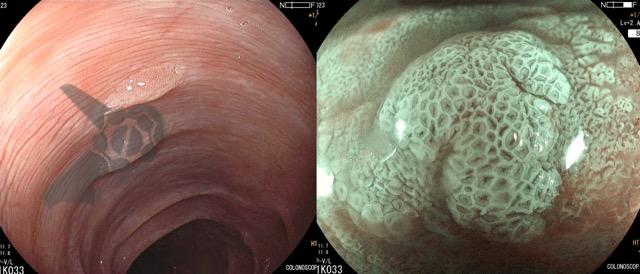
- Endoscopic characteristics:
- presence of a mucus cap
- Pale/whitish coloration.
- Type II-O (open) crypt pattern in magnifying chromoscopy.
3.3 – Sessile Serrated Lesions with Dysplasia (SSL-D)
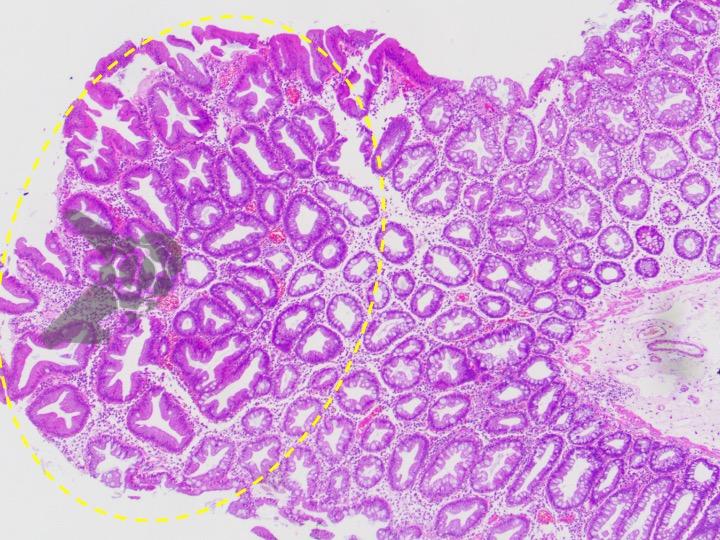
- According to their known carcinogenic potential, SSLs can originate dysplastic foci.
- This histological entity, called SSLD, represents a subgroup of SSLs.
- It is estimated that about 4–8% of SSLs contain dysplasia.
- At least three different morphological types of dysplasia have been described in SSLD:
- Intestinal dysplasia (similar to adenoma): rare.
- Serrated dysplasia: more common.
- Minimal deviation dysplasia: few changes compared to SSL and characteristic loss of MLH1.
- Endoscopically, these lesions usually present nodules on the surface.
- Signs such as (sub)pedunculated morphology, double elevation, central depression, and reddish hue are suspicious signs of dysplasia. [3]
- In magnifying chromoendoscopy, they exhibit an adenomatous pit pattern (Kudo type III, IV). [4]
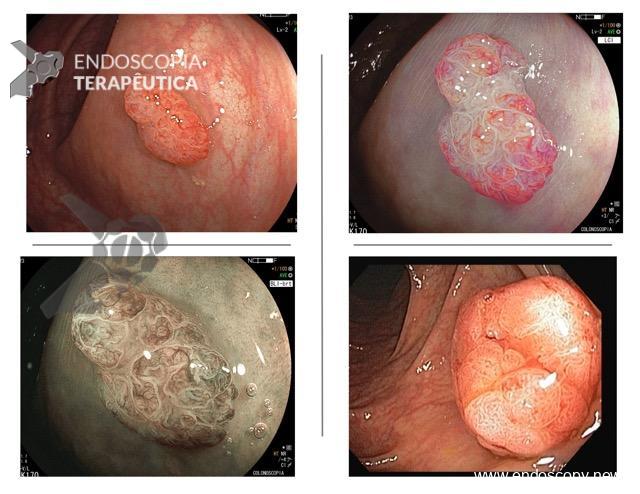
3.4 – Traditional Serrated Adenoma (TSA)
- Most common in the left colon.
- They are the rarest serrated colorectal lesions with a prevalence of less than 1%.
- Generally, TSA are larger than SSL and have a polypoid or pedunculated appearance.
- Histologically, they show distorted villous architecture and, in many cases, villi with bulbous tips.
- Both adenoma-like dysplasia and serrated dysplasia can be seen in TSA.
- The risk and speed of progression to carcinoma are unknown.
- On endoscopy, they look like reddish, protuberant or pedunculated lesions and, macroscopically, they have a “pine” or “coral” appearance.
Summary of Changes:
- Sessile serrated lesion (SSL) is the new term for lesions previously called sessile serrated adenoma (SSA). The clinical guidelines for the management of SSA apply to SSL.
- SSL with dysplasia is the term used for lesions previously called SSA with cytological dysplasia.
- Unclassified serrated adenoma has been introduced for rare polyps that are difficult to classify as SSL or TSA.
Summary of Histological Criteria for Sessile Lesions and Polyps:
- A single undisputed distorted crypt is sufficient to diagnose a sessile serrated lesion (SSL). Distortion of the crypt architecture can include horizontal growth along the muscularis mucosae, dilation of the crypt base and asymmetrical proliferation.
- Flat serrated lesions/polyps without a typical SSL-type crypt are diagnosed as hyperplastic polyps (HP) by exclusion. Mild symmetrical dilatation of the crypt and goblet cells at the base of the crypts are not sufficient to diagnose SSL.
- Stratification into low-grade and high-grade dysplasia is not recommended.
- The diagnosis of traditional serrated adenoma (TSA) requires two of the following characteristics:
- (1) slit-like serration;
- (2) tall eosinophilic cells with pencil nuclei;
- (3) ectopic crypt formations.
References:
- Mezzapesa M, Losurdo G, Celiberto F, Rizzi S, d’Amati A, Piscitelli D, Ierardi E, Di Leo A. Serrated Colorectal Lesions: An Up-to-Date Review from Histological Pattern to Molecular Pathogenesis. Int J Mol Sci. 2022 Apr 18;23(8):4461. doi: 10.3390/ijms23084461. PMID: 35457279; PMCID: PMC9032676.
- WHO Classification of Tumours Editorial Board . WHO Classification of Tumors: DIGESTIVE System Tumours. 5th ed. International Agency for Research on Cancer; Lyon, France: 2019
- Murakami T, Sakamoto N, Ritsuno H, Shibuya T, Osada T, Mitomi H, Yao T, Watanabe S. Distinct endoscopic characteristics of sessile serrated adenoma/polyp with and without dysplasia/carcinoma. Gastrointest Endosc. 2017 Mar;85(3):590-600. doi: 10.1016/j.gie.2016.09.018. Epub 2016 Sep 20. PMID: 27663716.
- Tate D.J., Jayanna M., Awadie H., Desomer L., Lee R., Heitman S.J., Sidhu M., Goodrick K., Burgess N.G., Mahajan H., et al. A standardized imaging protocol for the endoscopic prediction of dysplasia within sessile serrated polyps. Gastrointest. Endosc. 2018;87:222–231. doi: 10.1016/j.gie.2017.06.031.
How to cite this article
Martins BC e Tanigawa R. Colorectal Serrated Lesions. Endoscopy News, 2024 vol. 1. Available on: https://endoscopy.news/2024/01/09/colorectal-serrated-lesions
Professor Livre-Docente pela Faculdade de Medicina da Universidade de São Paulo
Médico Endoscopista do Instituto do Câncer do Estado de São Paulo (ICESP)
Médico Endoscopista do Hospital Alemão Oswaldo Cruz
Emerging Star pela WEO